Myfembree
Generic name: relugolix, estradiol and norethindrone acetate
Dosage form: tablets
Drug class: Sex hormone combinations
Medically reviewed by A Ras MD.
What is Myfembree?
Myfembree is a prescription medicine used to control heavy menstrual bleeding due to uterine fibroids in premenopausal women (before “change of life” or menopause). Myfembree contains relugolix, which reduces the amount of estrogen (and other hormones) produced by ovaries, estradiol (an estrogen) which may reduce the risk of bone loss, and norethindrone acetate (a progestin) which is necessary when women with a uterus (womb) take estrogen.
It is not known if Myfembree is safe and effective in children under 18 years of age.
Description
MYFEMBREE tablets for oral administration contain a fixed-dose combination of relugolix 40 mg, estradiol 1 mg, and norethindrone acetate 0.5 mg as active ingredients.
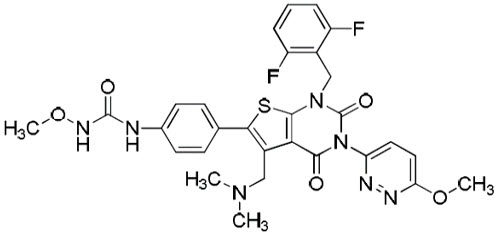
Relugolix is a non-peptide small molecule, GnRH receptor antagonist. It is a white to off white to slightly yellow solid and is sparingly soluble in water. The chemical name is N-(4-{1-[(2,6-difluorophenyl)methyl]-5-[(dimethylamino)methyl]-3-(6-methoxypyridazin-3-yl)-2,4-dioxo-1,2,3,4-tetrahydrothieno[2,3-d]pyrimidin-6-yl}phenyl)-N-methoxyurea with the empirical formula of C 29H 27F 2N 7O 5S and a molecular weight of 623.63. The structural formula is:
Estradiol (E2) is an estrogen with its chemical name as estra-1, 3, 5 (10)-triene-3, 17β-diol. The empirical formula of E2 is C 18H 24O 2 and a molecular weight of 272.4. The structural formula is:
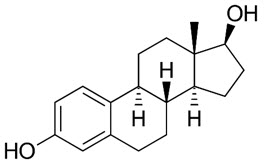
Estradiol is present as the hemihydrate (C 18H 24O 2∙½H 2O) which is a white or almost white crystalline powder.
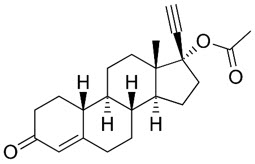
Norethindrone acetate (NETA), a progestin, is a white or yellowish-white crystalline powder. Its chemical name is 17-Hydroxy-19-nor-17α-pregn-4-en-20-yn-3-one acetate with the empirical formula of C 22H 28O 3 and a molecular weight of 340.5. The structural formula is:
Each MYFEMBREE (relugolix, estradiol, and norethindrone acetate) film-coated tablet contains the following inactive ingredients: hydroxypropyl cellulose, hypromellose, iron oxide yellow, lactose monohydrate, mannitol, magnesium stearate, sodium starch glycolate, titanium dioxide, and triacetin.
Mechanism of Action
MYFEMBREE is a combination of relugolix, estradiol (E2), and norethindrone acetate (NETA).
Relugolix is a non-peptide GnRH receptor antagonist that competitively binds to pituitary GnRH receptors, thereby reducing the release of luteinizing hormone (LH) and follicle-stimulating hormone (FSH), leading to decreased serum concentrations of the ovarian sex hormones estradiol and progesterone and reduced bleeding associated with uterine fibroids.
Estradiol acts by binding to nuclear receptors that are expressed in estrogen-responsive tissues. As a component of MYFEMBREE, the addition of exogenous estradiol may reduce the increase in bone resorption and resultant bone loss that can occur due to a decrease in circulating estrogen concentrations from relugolix alone.
Progestins such as norethindrone act by binding to nuclear receptors that are expressed in progesterone-responsive tissues. As a component of MYFEMBREE, norethindrone may protect the uterus from the potential adverse endometrial effects of unopposed estrogen
What is the most important information I should know about Myfembree?
Myfembree may cause serious side effects, including:
- cardiovascular conditions
- Myfembree may increase your chances of heart attack, stroke, or blood clots, especially if you are over 35 years of age, smoke, and have uncontrolled high blood pressure. Stop taking Myfembree and call your healthcare provider right away or go to the nearest hospital emergency room right away if you have:
- leg pain or swelling that will not go away
- sudden shortness of breath
- double vision, bulging of the eyes, sudden blindness, partial or complete
- pain or pressure in your chest, arm, or jaw
- sudden, severe headache unlike your usual headaches
- weakness or numbness in an arm or leg, or trouble speaking
- Myfembree may increase your chances of heart attack, stroke, or blood clots, especially if you are over 35 years of age, smoke, and have uncontrolled high blood pressure. Stop taking Myfembree and call your healthcare provider right away or go to the nearest hospital emergency room right away if you have:
- bone loss (decreased bone mineral density)
- While you are taking Myfembree, your estrogen levels may be low. Low estrogen levels can lead to bone mineral density loss.
- If you have bone loss on Myfembree, your bone density may improve after you stop taking Myfembree, but complete recovery may not occur. It is unknown if these bone changes could increase your risk for broken bones as you age. For this reason, you should not take Myfembree for more than 24 months.
- Your healthcare provider may order an X-ray test called a DXA scan to check your bone mineral density when you start taking Myfembree and periodically after you start.
- Your healthcare provider may advise you to take vitamin D and/or calcium supplements as part of a healthy lifestyle that promotes bone health. If you are also advised to take iron supplements, they should be taken at least two hours apart from your vitamin D or calcium supplements.
- effects on pregnancy
- Do not take Myfembree if you are trying to become pregnant or are pregnant. It may increase the risk of early pregnancy loss.
- If you think you are pregnant, stop taking Myfembree right away and call your healthcare provider.
- If you become pregnant while taking Myfembree, you are encouraged to enroll in the Pregnancy Registry. The purpose of the pregnancy registry is to collect information about the health of you and your baby. Talk to your healthcare provider or call 1-(855) 428-0707.
- Myfembree can decrease your menstrual bleeding or result in no menstrual bleeding at all, making it hard to know if you are pregnant. Watch for other signs of pregnancy such as breast tenderness, weight gain and nausea.
- Myfembree does not prevent pregnancy. You will need to use effective methods of birth control while taking Myfembree and for 1 week after you stop taking Myfembree. Examples of effective methods can include condoms or spermicide, which do not contain hormones.
- Do not take hormonal birth control such as birth control pills, because they may increase your side effects and Myfembree may not work as well.
Talk to your healthcare provider about which birth control to use during treatment with Myfembree. Your healthcare provider may change the birth control you were on before you start taking Myfembree.
Who should not take Myfembree?
Do not take Myfembree if you:
- have or have had:
- blood clots in your legs (deep vein thrombosis), lungs (pulmonary embolism), or eyes (retinal thrombosis)
- stroke or heart attack
- a problem that makes your blood clot more than normal
- blood circulation disorders
- certain heart valve problems or heart rhythm abnormalities that can cause blood clots to form in the heart
- high blood pressure not well controlled by medicine
- diabetes with kidney, eye, nerve, or blood vessel damage
- certain kinds of severe migraine headaches with aura, numbness, weakness or changes in vision or migraine headaches if you are over age 35
- breast cancer or any cancer that is sensitive to female hormones
- osteoporosis
- vaginal bleeding that has not been diagnosed. Your healthcare provider should check any unexplained vaginal bleeding to find out the cause.
- liver problems including liver disease
- smoke and are over 35 years old
- have had a serious allergic reaction with symptoms that included swelling of your face, lips, mouth or tongue, trouble breathing, skin rashes, redness, or swelling or an allergic reaction to relugolix, estradiol, norethindrone or any of the ingredients in Myfembree.
See the end of this Patient Package Insert for a complete list of ingredients in Myfembree.
What should I tell my healthcare provider before taking Myfembree?
Before you take Myfembree, tell your healthcare provider about all of your medical conditions including if you:
- have or have had:
- broken bones or other conditions that may cause bone problems.
- depression, mood swings, or suicidal thoughts or behavior.
- yellowing of the skin or eyes (jaundice) or jaundice caused by pregnancy (cholestasis of pregnancy).
- are scheduled for surgery or will be on bed rest. Myfembree may increase your risk of blood clots after surgery. Your healthcare provider may advise you to stop taking Myfembree before you have surgery. Talk to your healthcare provider about when to stop Myfembree before surgery and when to restart Myfembree after surgery.
- are pregnant or think you may be pregnant or just had a baby.
- are breastfeeding. Myfembree may pass into your breast milk. Talk to your healthcare provider about the best way to feed your baby if you take Myfembree.
Tell your healthcare provider about all the medicines you take, including prescription, over-the-counter medicines, vitamins, and herbal supplements.
Women on thyroid or cortisol replacement therapy may need increased doses of the hormone.
Know the medicines you take. Keep a list of your medicines with you to show to your healthcare provider and pharmacist when you get a new medicine.
How should I take Myfembree?
- Take Myfembree exactly as your healthcare provider tells you to take it.
- Take Myfembree 1 time each day at about the same time with or without food.
- If you have to take oral P-gp inhibitors, take Myfembree first and wait at least 6 hours before taking the P-gp inhibitor. Ask your healthcare provider if you are not sure if you are taking this type of medicine.
- Your healthcare provider may give you a pregnancy test before you start taking Myfembree.
- You should begin Myfembree as soon as possible after your period begins, but no later than 7 days after your period has started. If you start Myfembree on another day, your period may become heavy or irregular for the first month after starting treatment, but bleeding should decrease after this time.
- If you take too much Myfembree, call your healthcare provider or go to the nearest hospital emergency room right away.
- If you miss a dose, take the missed dose as soon as you remember on that day, and then take Myfembree at the usual time the next day.
- Do not take 2 doses at once to make up for the missed dose. If you do not remember until you are due for Myfembree on the next day, do not make up for the missed dose.
What are the possible side effects of Myfembree?
Myfembree may cause serious side effects including:
- See “What is the most important information I should know about Myfembree?”
- suicidal thoughts, suicidal behavior, and worsening of mood. Call your healthcare provider or get emergency medical help right away if you have any of these symptoms, especially if they are new, worse, or bother you:
- thoughts about suicide or dying
- attempts to commit suicide
- new or worse depression
- new or worse anxiety
- other unusual changes in behavior or mood
Pay attention to any changes, especially sudden changes in your mood, behaviors, thoughts, or feelings.
- abnormal liver tests. Call your healthcare provider right away if you have any of these signs and symptoms of liver problems:
- jaundice
- dark amber-colored urine
- feeling tired (fatigue or exhaustion)
- nausea and vomiting
- generalized swelling
- right upper stomach area (abdomen) pain
- bruising easily
- gallbladder problems (cholestasis), especially if you had cholestasis of pregnancy.
- high blood pressure. See your healthcare provider to check your blood pressure regularly.
- uterine fibroid prolapse or expulsion. Fibroids can come out completely or partially through the vagina. Call your healthcare provider right away if you have increased bleeding from the vagina, which can be serious, or cramping, while taking Myfembree.
- hair loss (alopecia). Hair loss and hair thinning can happen while taking Myfembree. It is not known if this hair loss or hair thinning stops after you stop taking Myfembree or is reversible. Talk to your healthcare provider if this is a concern for you.
- increases in the blood sugar, cholesterol and fat (triglycerides) levels in your blood.
- changes in laboratory tests including thyroid, steroid, hormone, cholesterol, and blood clotting tests.
The most common side effects of Myfembree include:
- hot flushes
- increased sweating
- night sweats
- abnormal vaginal bleeding (bleeding that lasts too long, is too much, or is unexpected)
- hair loss or hair thinning
- decreased interest in sex
These are not all the possible side effects of Myfembree. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
General information about the safe and effective use of Myfembree
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet. Do not use Myfembree for a condition for which it was not prescribed. Do not give Myfembree to other people, even if they have the same symptoms that you have. It may harm them. You can ask your healthcare provider or pharmacist for information about Myfembree that is written for health professionals.
How should I store Myfembree?
- Store Myfembree at room temperature between 59°F to 86°F (15°C to 30°C).
- Dispose of unused medicines through community take-back disposal programs when available. If no community take-back disposal program is available go to www.fda.gov/drugdisposal for information on how to dispose of Myfembree the right way.
- Do not flush Myfembree down the toilet.
- Do not keep medicine that is out of date or that you no longer need.
- Keep Myfembree and all medicines out of the reach of children
What are the ingredients in Myfembree?
Active ingredient: relugolix, estradiol, and norethindrone acetate
Inactive ingredients: lactose monohydrate, mannitol, sodium starch glycolate, hydroxypropyl cellulose, magnesium stearate, hypromellose, titanium dioxide, triacetin, iron oxide yellow.
Label
PRINCIPAL DISPLAY PANEL – 28 TABLET BOTTLE LABEL
- NDC 72974-415-01
Rx only - Myfembree ®
- (relugolix, estradiol, and
norethindrone acetate) tablets
40 mg, 1 mg, 0.5 mg - 28 tablets
SRC: NLM .