Mirena
Generic name: levonorgestrel intrauterine system
Drug classes: Contraceptives, Progestins
Medically reviewed by A Ras MD.
What is Mirena?
Mirena is a hormone-releasing system placed in your uterus by your healthcare provider to prevent pregnancy for up to 7 years. Mirena can also be used to decrease menstrual blood loss for up to 5 years in women who have heavy menstrual flow and who also want to use a birth control method that is placed in the uterus to prevent pregnancy.
Mirena can be removed by your healthcare provider at any time.
Mirena can be used whether or not you have given birth to a child.
Mirena is a small flexible plastic T-shaped system that slowly releases a progestin hormone called levonorgestrel (LNG) that is often used in birth control pills. Because Mirena releases LNG into your uterus, only small amounts of the hormone enter your blood. Mirena does not contain estrogen.
Two thin threads are attached to the stem (lower end) of Mirena. The threads are the only part of Mirena you can feel when Mirena is in your uterus; however, unlike a tampon string, the threads do not extend outside your body.

Mirena is small

Mirena is flexible
Description
Mirena (levonorgestrel-releasing intrauterine system) contains 52 mg of LNG, a progestin, and is intended to provide an initial release rate of approximately 20 mcg/day of LNG.
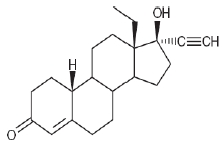
Levonorgestrel USP, (-)-13-Ethyl-17-hydroxy-18,19-dinor-17α-pregn-4-en-20-yn-3-one, the active ingredient in Mirena, has a molecular weight of 312.4, a molecular formula of C21H28O2, and the following structural formula:
11.1 Mirena
Mirena consists of a T-shaped polyethylene frame (T-body) with a steroid reservoir (hormone elastomer core) around the vertical stem. The white T-body has a loop at one end of the vertical stem and two horizontal arms at the other end. The reservoir consists of a white or almost white cylinder, made of a mixture of LNG and silicone (polydimethylsiloxane), containing a total of 52 mg LNG. The reservoir is covered by a semi-opaque silicone membrane, composed of polydimethylsiloxane and colloidal silica. The T-body is 32 mm in both the horizontal and vertical directions. The polyethylene of the T-body is compounded with barium sulfate, which makes it radiopaque. A monofilament brown polyethylene removal thread is attached to a loop at the end of the vertical stem of the T-body. The polyethylene of the removal thread contains iron oxide as a colorant .
The components of Mirena, including its packaging, are not manufactured using natural rubber latex.
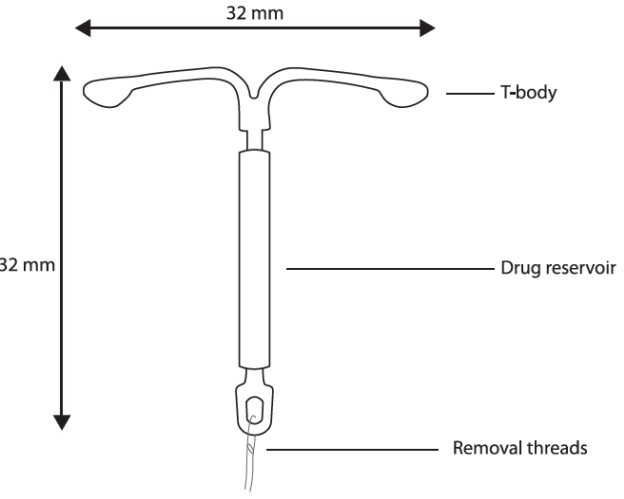
Figure 10. Mirena
11.2 Inserter
Mirena is packaged sterile within an inserter. The inserter (Figure 11), which is used for insertion of Mirena into the uterine cavity, consists of a symmetric two-sided body and slider that are integrated with flange, lock, pre-bent insertion tube and plunger. The outer diameter of the insertion tube is 4.4 mm. The vertical stem of Mirena is loaded in the insertion tube at the tip of the inserter. The arms are pre-aligned in the horizontal position. The removal threads are contained within the insertion tube and handle. Once Mirena has been placed, the inserter is discarded.
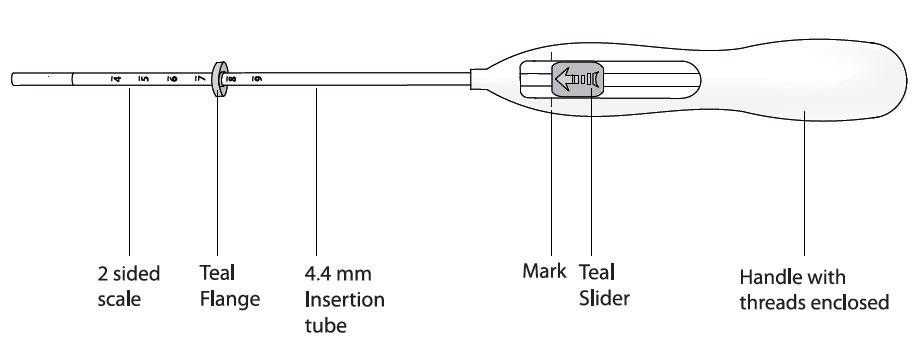
Figure 11. Diagram of Inserter
Mechanism of Action
The local mechanism by which continuously released LNG contributes to the contraceptive effectiveness of Mirena has not been conclusively demonstrated. Studies of Mirena and similar LNG IUS prototypes have suggested several mechanisms that prevent pregnancy: thickening of cervical mucus preventing passage of sperm into the uterus, inhibition of sperm capacitation or survival, and alteration of the endometrium.
What if I need birth control for more than 7 years?
Mirena must be removed after 7 years. Your healthcare provider can place a new Mirena during the same office visit if you choose to continue using Mirena.
What if I need treatment for heavy menstrual flow for more than 5 years?
For continued treatment of heavy menstrual flow after 5 years, your healthcare provider can remove Mirena and place a new Mirena during the same office visit.
What if I want to stop using Mirena?
Mirena is intended for use up to 7 years, but you can stop using Mirena at any time by asking your healthcare provider to remove it. You could become pregnant as soon as Mirena is removed, so you should use another method of birth control if you do not want to become pregnant. Talk to your healthcare provider about the best birth control methods for you, because your new method may need to be started 7 days before Mirena is removed to prevent pregnancy.
What if I change my mind about birth control and want to become pregnant in less than 7 years?
Your healthcare provider can remove Mirena at any time. You may become pregnant as soon as Mirena is removed. About 8 out of 10 women who want to become pregnant will become pregnant sometime in the first year after Mirena is removed.
How does Mirena work?
Mirena may work in several ways including thickening cervical mucus, inhibiting sperm movement, reducing sperm survival, and thinning the lining of your uterus. It is not known exactly how these actions work together to prevent pregnancy.
Mirena can cause your menstrual bleeding to be less by thinning the lining of the uterus.

How well does Mirena work for contraception?
The following chart shows the chance of getting pregnant for women who use different methods of birth control. Each box on the chart contains a list of birth control methods that are similar in effectiveness. The most effective methods are at the top of the chart. The box on the bottom of the chart shows the chance of getting pregnant for women who do not use birth control and are trying to get pregnant.
Mirena, an intrauterine device (IUD), is in the box at the top of the chart.

How well does Mirena work for heavy menstrual bleeding?
In the clinical trial performed in women with heavy menstrual bleeding and treated with Mirena, almost 9 out of 10 were treated successfully and their blood loss was reduced by more than half.
Who might use Mirena?
You might choose Mirena if you:
- want long-term birth control that provides a low chance of getting pregnant (less than 1 in 100)
- want birth control that works continuously for up to 7 years
- want birth control that is reversible
- want a birth control method that you do not need to take daily
- want treatment for heavy periods up to 5 years and are willing to use a birth control method that is placed in the uterus
- want birth control that does not contain estrogen
What is the most important information I should know about Mirena?
Mirena does not protect against HIV infection (AIDS) and other sexually transmitted infections (STIs).
Who should not use Mirena?
Do not use Mirena if you:
- are or might be pregnant; Mirena cannot be used as an emergency contraceptive
- have a serious pelvic infection called pelvic inflammatory disease (PID) or have had PID in the past unless you have had a normal pregnancy after the infection went away
- have an untreated genital infection now
- have had a serious pelvic infection in the past 3 months after a pregnancy
- can get infections easily. For example, if you:
- have multiple sexual partners or your partner has multiple sexual partners
- have problems with your immune system
- use or abuse intravenous drugs
- have or suspect you might have cancer of the uterus or cervix
- have bleeding from the vagina that has not been explained
- have liver disease or liver tumor
- have breast cancer or any other cancer that is sensitive to progestin (a female hormone), now or in the past
- have an intrauterine device in your uterus already
- have a condition of the uterus that changes the shape of the uterine cavity, such as large fibroid tumors
- are allergic to levonorgestrel, silicone, polyethylene, silica, barium sulfate or iron oxide
What should I tell my healthcare provider before using Mirena?
Before having Mirena placed, tell your healthcare provider about all of your medical conditions including if you:
- have any of the conditions listed above
- have had a heart attack
- have had a stroke
- were born with heart disease or have problems with your heart valves
- have problems with blood clotting or take medicine to reduce clotting
- have high blood pressure
- recently had a baby or if you are breastfeeding
- have severe headaches or migraine headaches
- have AIDS, HIV, or any other sexually transmitted infection
Tell your healthcare provider about all of the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements.
How should I use Mirena?
Mirena is placed by your healthcare provider during an in-office visit or immediately after giving birth.
First, your healthcare provider will examine your pelvis to find the exact position of your uterus. Your healthcare provider will then clean your vagina and cervix with an antiseptic solution and slide a slim plastic tube containing Mirena through the cervix into your uterus. Your healthcare provider will then remove the plastic tube and leave Mirena in your uterus. Your healthcare provider will cut the threads to the right length
You may experience pain, bleeding or dizziness during and after placement. If your symptoms do not pass within 30 minutes after placement, Mirena may not have been placed correctly. Your healthcare provider will examine you to see if Mirena needs to be removed or replaced.
Should I check that Mirena is in place?
Yes, you should check that Mirena is in proper position by feeling the removal threads. It is a good habit to do this 1 time a month. Your healthcare provider should teach you how to check that Mirena is in place. First, wash your hands with soap and water. You can check by reaching up to the top of your vagina with clean fingers to feel the removal threads. Do not pull on the threads.
If you feel more than just the threads or if you cannot feel the threads, Mirena may not be in the right position and may not prevent pregnancy. Avoid intercourse or use non-hormonal back-up birth control (such as condoms and spermicide) and ask your healthcare provider to check that Mirena is still in the right place.
How soon after placement of Mirena should I return to my healthcare provider?
Call your healthcare provider if you have any questions or concerns (see “When should I call my healthcare provider?”). Otherwise, you should return to your healthcare provider for a follow-up visit 4 to 6 weeks after Mirena is placed to make sure that Mirena is in the right position.
Can I use tampons or menstrual cups with Mirena?
Yes, tampons or menstrual cups may be used with Mirena. Change tampons or menstrual cups with care to avoid pulling the threads of Mirena. If you think you may have pulled Mirena out of place, avoid intercourse or use a non-hormonal back-up birth control (such as condoms or spermicide), and contact your healthcare provider.
What if I become pregnant while using Mirena?
Call your healthcare provider right away if you think you are pregnant.If you get pregnant while using Mirena, you may have an ectopic pregnancy. This means that the pregnancy is not in the uterus. Unusual vaginal bleeding or abdominal pain may be a sign of ectopic pregnancy.
Ectopic pregnancy is a medical emergency that often requires surgery. Ectopic pregnancy can cause internal bleeding, infertility, and even death.
There are also risks if you get pregnant while using Mirena and the pregnancy is in the uterus. Severe infection, miscarriage, premature delivery, and even death can occur with pregnancies that continue with an intrauterine device (IUD). Because of this, your healthcare provider may try to remove Mirena, even though removing it may cause a miscarriage. If Mirena cannot be removed, talk with your healthcare provider about the benefits and risks of continuing the pregnancy and possible effects of the hormone on your unborn baby.
If you continue your pregnancy, see your healthcare provider regularly. Call your healthcare provider right away if you get flu-like symptoms, fever, chills, cramping, pain, bleeding, vaginal discharge, or fluid leaking from your vagina. These may be signs of infection.
How will Mirena change my periods?
For the first 3 to 6 months, your period may become irregular and the number of bleeding days may increase. You may also have frequent spotting or light bleeding, and some women have heavy bleeding during this time. You may also have cramping during the first few weeks. After you have used Mirena for a while, the number of bleeding and spotting days is likely to lessen. For some women, periods will stop altogether. When Mirena is removed, your menstrual periods should return.
In some women with heavy bleeding, the total blood loss per cycle progressively decreases with continued use. The number of spotting and bleeding days may initially increase but then typically decreases in the months that follow.
Is it safe to breastfeed while using Mirena?
You may use Mirena when you are breastfeeding. Mirena is not likely to affect the quality or amount of your breast milk or the health of your nursing baby. However, isolated cases of decreased milk production have been reported. The risk of Mirena going into the wall of the uterus (becoming embedded) or going through the wall of the uterus is increased if Mirena is inserted while you are breastfeeding.
Will Mirena interfere with sexual intercourse?
You and your partner should not feel Mirena during intercourse. Mirena is placed in the uterus, not in the vagina. Sometimes your partner feels the threads. If this occurs, or if you or your partner experience pain during sex, talk with your healthcare provider.
What are the possible side effects of using Mirena?
Mirena can cause serious side effects including:
- Ectopic pregnancy and intrauterine pregnancy risks. There are risks if you become pregnant while using Mirena (see “What if I become pregnant while using Mirena?”).
- Life-threatening Infection. Life-threatening infection can occur within the first few days after Mirena is placed. Call your healthcare provider immediately if you develop severe pain or fever shortly after Mirena is placed.
- Pelvic Inflammatory Disease (PID). Some IUD users get a serious pelvic infection called pelvic inflammatory disease. PID is usually sexually transmitted. You have a higher chance of getting PID if you or your partner have sex with other partners. PID can cause serious problems such as infertility, ectopic pregnancy or pelvic pain that does not go away. PID is usually treated with antibiotics. More serious cases of PID may require surgery including removal of the uterus (hysterectomy). In rare cases, infections that start as PID can even cause death.
Tell your healthcare provider right away if you have any of these signs of PID: long-lasting or heavy bleeding, unusual vaginal discharge, low abdominal (stomach area) pain, painful sex, chills, fever, genital lesions or sores. - Perforation. Mirena may go into the wall of the uterus (become embedded) or go through the wall of the uterus. This is called perforation. If this occurs, Mirena may no longer prevent pregnancy. If perforation occurs, Mirena may move outside the uterus and can cause internal scarring, infection, or damage to other organs, and you may need surgery to have Mirena removed. Excessive pain or vaginal bleeding during placement of Mirena, pain or bleeding that gets worse after placement, or not being able to feel the threads may happen with perforation. The risk of perforation is increased if Mirena is inserted while you are breastfeeding, or if you have recently given birth.
- Expulsion. Mirena may come out by itself. This is called expulsion. Excessive pain or vaginal bleeding during placement of Mirena, pain or bleeding that gets worse after placement, or not being able to feel the threads may happen with expulsion. You may become pregnant if Mirena comes out. If you think that Mirena has come out, avoid intercourse or use a non-hormonal back-up birth control (such as condoms and spermicide) and call your healthcare provider. The risk of expulsion is increased with insertion right after delivery or second-trimester abortion.
Common side effects of Mirena include:
- Pain, bleeding or dizziness during and after placement. If these symptoms do not stop 30 minutes after placement, Mirena may not have been placed correctly. Your healthcare provider will examine you to see if Mirena needs to be removed or replaced.
- Changes in bleeding. You may have bleeding and spotting between menstrual periods, especially during the first 3 to 6 months. Sometimes the bleeding is heavier than usual at first. However, the bleeding usually becomes lighter than usual and may be irregular. Call your healthcare provider if the bleeding remains heavier than usual or increases after it has been light for a while.
- Missed menstrual periods. About 2 out of 10 women stop having periods after 1 year of Mirena use. If you have any concerns that you may be pregnant while using Mirena, do a urine pregnancy test and call your healthcare provider. If you do not have a period for 6 weeks during Mirena use, call your healthcare provider. When Mirena is removed, your menstrual periods should return.
- Cysts on the ovary. Some women using Mirena develop a painful cyst on the ovary. These cysts usually disappear on their own in 2 to 3 months. However, cysts can cause pain and sometimes cysts will need surgery.
Other common side effects include:
- abdominal pain/pelvic pain
- infection of the outer part of your vagina (vulvovaginitis)
- headache or migraines
- vaginal discharge
These are not all of the possible side effects with Mirena. For more information, ask your healthcare provider.
Call your healthcare provider for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. You may also report side effects to Bayer Healthcare Pharmaceuticals at 1-888-842-2937.
After Mirena has been placed, when should I call my healthcare provider?
If Mirena is accidentally removed and you had vaginal intercourse within the preceding week, you may be at risk of pregnancy, and you should talk to a healthcare provider.
Call your healthcare provider if you have any concerns about Mirena. Be sure to call if you:
- think you are pregnant
- have pelvic pain or pain during sex
- have unusual vaginal discharge or genital sores
- have unexplained fever, flu-like symptoms or chills
- might be exposed to sexually transmitted infections (STIs)
- are concerned that Mirena may have been expelled (came out)
- cannot feel Mirena’s threads
- develop very severe or migraine headaches
- have yellowing of the skin or whites of the eyes. These may be signs of liver problems.
- have had a stroke or heart attack
- become HIV positive or your partner becomes HIV positive
- have severe vaginal bleeding or bleeding that lasts a long time or concerns you
General advice about the safe and effective use of Mirena
Medicines are sometimes prescribed for purposes other than those listed in patient information leaflets. If you would like more information, talk with your healthcare provider. You can ask your healthcare provider for information about Mirena that is written for health professionals.
What are the ingredients in Mirena?
Active ingredient: levonorgestrel
Inactive ingredients: silicone, polyethylene, silica, barium sulfate, iron oxide
Label
PRINCIPAL DISPLAY PANEL
- Mirena (levonorgestrel-releasing intrauterine system) Carton
- NDC 50419-423-01
- 1 Sterile Unit
- NEW contains updated single-handed inserter with no removable threads
- IMPORTANT: To be inserted in the uterus by a trained healthcare provider. Mirena cannot be reloaded.. See physician insert for detailed instructions for use.
- Mirena
- (levonorgestrel-releasing intrauterine system)
- Rx only
- — 52 mg levonorgestrel
- — 1 sterile unit
- — intrauterine use

SRC: NLM .